Microsurgical testicular sperm extraction (microTESE) is a specialized procedure offering hope for men facing infertility due to azoospermia, with Cyprus IVF Centre leading the way in advanced fertility solutions. For couples struggling to conceive, this innovative technique can be a game-changer, retrieving viable sperm directly from the testicles to support assisted reproductive technologies like IVF or ICSI. In this article, we’ll explore the intricacies of microTESE, when it’s needed, how it’s performed, what to expect afterward, and how Cyprus IVF Centre is making this procedure accessible. We’ll also compare it to TESA and TESE, helping you understand which sperm retrieval method may suit your needs.
Understanding Microsurgical Testicular Sperm Extraction
Microsurgical testicular sperm extraction, often abbreviated as microTESE, is a cutting-edge procedure designed to retrieve sperm from the testicles of men who have no sperm in their ejaculate, a condition known as azoospermia. Unlike traditional sperm retrieval methods, microTESE uses a high-powered microscope to identify and extract sperm-producing tubules with precision, increasing the chances of finding viable sperm while minimizing tissue damage. This makes it a preferred choice for complex cases of male infertility.
The procedure is typically recommended for men with non-obstructive azoospermia, where sperm production is impaired due to genetic conditions, hormonal imbalances, or testicular injury. By targeting specific areas of the testicle, microTESE offers hope for couples pursuing in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI), enabling them to use their own genetic material rather than relying on donor sperm.
At Cyprus IVF Centre, microTESE is performed by experienced specialists who combine advanced technology with compassionate care, ensuring patients receive personalized treatment plans tailored to their unique fertility challenges. The clinic’s commitment to excellence has made it a trusted destination for couples worldwide seeking effective sperm retrieval solutions.
When Is Sperm Retrieval from Testicles Necessary?
Sperm retrieval from the testicles becomes necessary under specific circumstances, primarily when a man’s ejaculate lacks sperm or contains insufficient sperm for fertilization. Below are the key conditions that may warrant microsurgical testicular sperm extraction or other retrieval methods:
- Non-Obstructive Azoospermia: This occurs when the testicles produce little to no sperm due to factors like genetic disorders (e.g., Klinefelter syndrome), chemotherapy, radiation, or testicular failure. MicroTESE is particularly effective here, as it targets areas with potential sperm production.
- Obstructive Azoospermia: In cases where sperm production is normal but blockages in the reproductive tract (e.g., from a vasectomy, infections, or congenital absence of the vas deferens) prevent sperm from reaching the ejaculate, retrieval procedures like microTESE or TESA can bypass the obstruction.
- Failed Vasectomy Reversal: Men who undergo unsuccessful vasectomy reversals may require sperm retrieval to achieve pregnancy through IVF or ICSI.
- Hormonal Imbalances: Conditions like low testosterone or elevated follicle-stimulating hormone (FSH) levels can impair sperm production, necessitating direct retrieval from the testicles.
- Previous Testicular Trauma or Surgery: Injuries or surgeries affecting the testicles may reduce sperm output, making microTESE a viable option to locate viable sperm.
For couples facing these challenges, Cyprus IVF Centre offers comprehensive diagnostic evaluations to determine the underlying cause of infertility and recommend the most suitable sperm retrieval approach. By addressing both medical and emotional aspects, the clinic ensures patients feel supported throughout their journey.
How Is MicroTESE Performed? A Step-by-Step Guide
The microTESE procedure is a meticulous process requiring surgical expertise and advanced equipment. Here’s a detailed look at how microsurgical testicular sperm extraction is carried out, particularly at Cyprus IVF Centre:
- Pre-Procedure Consultation: Before undergoing microTESE, patients meet with a fertility specialist to review medical history, hormone levels, and semen analysis results. At Cyprus IVF Centre, this consultation includes a thorough assessment to confirm microTESE as the best option and to discuss expectations.
- Anesthesia Administration: The procedure is performed under general anesthesia or local anesthesia with sedation to ensure patient comfort. Cyprus IVF Centre prioritizes safety, with an experienced anesthesiologist monitoring the patient throughout.
- Surgical Incision: A small incision, typically 3–4 cm, is made in the midline of the scrotum to access the testicles. The incision is carefully planned to minimize scarring and promote rapid healing.
- Microscopic Examination: Using a high-powered operating microscope, the surgeon examines the testicular tissue to identify seminiferous tubules likely to contain sperm. This precision distinguishes microTESE from other methods, as it targets only the most promising areas.
- Tissue Extraction: Tiny samples of tissue are removed from the identified tubules and sent to an embryologist in the lab. The embryologist examines the samples under a microscope to confirm the presence of viable sperm.
- Closure and Recovery: Once sufficient tissue is collected, the incision is closed with dissolvable stitches. The scrotum’s natural healing properties ensure minimal discomfort, and patients are typically discharged the same day.
At Cyprus IVF Centre, the microTESE procedure is conducted in a state-of-the-art operating room, with a focus on precision and patient safety. The clinic’s embryologists work in real-time to assess sperm quality, ensuring the best possible outcomes for subsequent IVF or ICSI cycles.
What Happens During MicroTESE? Inside the Operating Room
During microsurgical testicular sperm extraction, the operating room is a hub of precision and collaboration. The surgical team, including a urologist specializing in male infertility, an anesthesiologist, and an embryologist, works together to maximize the procedure’s success. Here’s what unfolds:
- Sterile Environment: The procedure takes place in a sterile surgical suite to prevent infections. Cyprus IVF Centre adheres to international standards for cleanliness and safety.
- Microscope-Guided Surgery: The urologist uses a high-magnification microscope (up to 25x) to inspect the testicular tissue. This allows them to distinguish between tubules with active sperm production and those that are inactive, reducing unnecessary tissue removal.
- Real-Time Sperm Analysis: As tissue samples are extracted, they’re immediately handed to the embryologist, who examines them for sperm. This real-time feedback helps the surgeon decide whether additional samples are needed.
- Minimally Invasive Approach: Unlike older methods, microTESE minimizes damage to the testicle’s blood vessels and surrounding structures, preserving testicular function and reducing recovery time.
- Patient Monitoring: The anesthesiologist ensures the patient remains stable, adjusting sedation or anesthesia as needed for comfort and safety.
The procedure typically lasts 1–2 hours, depending on the complexity of the case. At Cyprus IVF Centre, the integration of advanced microscopy and skilled professionals ensures microTESE is performed with the highest level of care, offering hope to men with even the most challenging infertility diagnoses.
What to Expect After MicroTESE: Recovery and Next Steps
Recovery from microsurgical testicular sperm extraction is generally swift, thanks to the procedure’s minimally invasive nature. Here’s what patients can expect post-procedure, along with the next steps in their fertility journey:
- Immediate Post-Operative Period: After microTESE, patients are monitored in a recovery room for a few hours before being discharged. Mild discomfort or swelling in the scrotum is normal and can be managed with prescribed pain relievers and ice packs.
- Healing Process: The scrotum heals quickly, with most patients resuming light activities within 2–3 days. Cyprus IVF Centre provides detailed aftercare instructions, including avoiding heavy lifting, strenuous exercise, and sexual activity for about 10 days to prevent complications.
- Sperm Analysis Results: The embryologist’s examination of the tissue samples takes 10–14 hours. Patients are informed whether viable sperm were found, which determines the next steps. If sperm are retrieved, they can be used immediately for IVF/ICSI or frozen for future cycles.
- Follow-Up Care: A follow-up appointment is scheduled within a week to check the incision site and discuss results. Cyprus IVF Centre offers ongoing support, guiding patients through the IVF process if sperm retrieval is successful.
- Emotional Support: Undergoing microTESE can be emotionally taxing. The clinic’s counselors are available to help patients and their partners cope with the uncertainties and plan their path forward.
If no sperm are found, the team at Cyprus IVF Centre discusses alternative options, such as donor sperm or additional diagnostic tests, ensuring couples have a clear understanding of their choices. The clinic’s holistic approach prioritizes both physical and emotional well-being during this critical time.
How Cyprus IVF Centre Enhances Access to MicroTESE
Cyprus IVF Centre is dedicated to making microsurgical testicular sperm extraction accessible to patients worldwide, combining affordability, expertise, and patient-centered care. Here’s how the clinic stands out:
- Affordable Treatment Options: Fertility treatments can be costly, but Cyprus IVF Centre offers competitive pricing for microTESE without compromising quality. Transparent cost structures help patients plan their journey with confidence.
- World-Class Facilities: The clinic is equipped with cutting-edge technology, including high-powered microscopes and advanced embryology labs, ensuring optimal outcomes for microTESE and subsequent IVF/ICSI procedures.
- Experienced Specialists: The team includes urologists and embryologists with extensive experience in male infertility, trained to perform microTESE with precision and care. Their expertise contributes to high sperm retrieval rates, even in challenging cases.
- Streamlined International Care: Recognizing that many patients travel from abroad, Cyprus IVF Centre provides seamless coordination, including virtual consultations, travel assistance, and multilingual support, making the process stress-free.
- Personalized Treatment Plans: Every patient receives a tailored approach, with microTESE integrated into a broader fertility strategy that considers both partners’ needs, optimizing the chances of a successful pregnancy.
- Commitment to Compliance: The clinic adheres to international medical standards and ethical guidelines, ensuring all procedures, including microTESE, are performed responsibly and transparently, aligning with regulations in regions like the UK and Northern Ireland.
By focusing on accessibility and quality, Cyprus IVF Centre empowers couples to pursue their dreams of parenthood, offering hope through advanced techniques like microsurgical testicular sperm extraction.
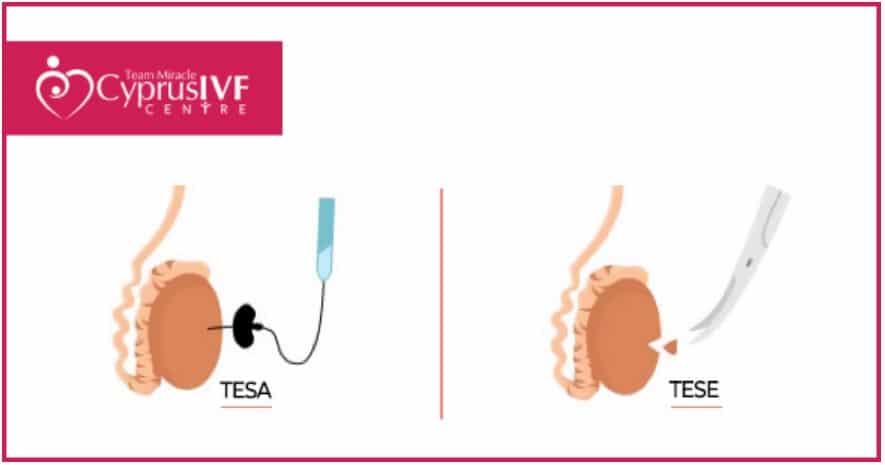
What Is TESA? Understanding Testicular Sperm Aspiration
Testicular sperm aspiration (TESA) is another sperm retrieval method used when no sperm are present in the ejaculate. Unlike microTESE, which involves surgical tissue extraction, TESA is less invasive, using a fine needle to aspirate sperm directly from the testicle. Here’s a closer look:
- Procedure Overview: Performed under local anesthesia, TESA involves inserting a needle into the testicle to draw out fluid and tissue containing sperm. The sample is then analyzed in the lab to identify viable sperm for IVF/ICSI.
- Best Candidates: TESA is often recommended for men with obstructive azoospermia, where sperm production is normal but blocked from reaching the ejaculate. It’s less effective for non-obstructive azoospermia, where microTESE is preferred.
- Advantages: TESA is quicker (typically 30 minutes) and requires no surgical incision, leading to a faster recovery. It’s also less costly than microTESE, making it an attractive option for suitable candidates.
- Limitations: Because TESA collects smaller samples blindly, it may yield fewer sperm or fail in cases of low sperm production, particularly in non-obstructive azoospermia.
At Cyprus IVF Centre, TESA is offered as part of a comprehensive suite of sperm retrieval options, with specialists guiding patients to the most appropriate method based on their diagnosis and fertility goals.
TESA vs. TESE: Which Is Better for Sperm Extraction?
Comparing TESA and TESE (testicular sperm extraction) with microTESE helps clarify which procedure is best for specific situations. TESE involves surgically removing small pieces of testicular tissue through an incision, similar to microTESE, but without the microscope-guided precision. Here’s a breakdown:
- Invasiveness:
- TESA: Least invasive, using a needle with no incision.
- TESE: Moderately invasive, requiring a small incision and tissue removal.
- MicroTESE: Most precise, using a microscope to minimize tissue damage despite a similar incision.
- Sperm Retrieval Rates:
- TESA: Effective for obstructive azoospermia (70–90% success) but less reliable for non-obstructive azoospermia (20–30% success).
- TESE: Higher retrieval rates than TESA for non-obstructive azoospermia (40–50%) but less precise than microTESE.
- MicroTESE: Offers the highest retrieval rates for non-obstructive azoospermia (50–70%), thanks to targeted tissue selection.
- Recovery Time:
- TESA: 1–2 days, with minimal discomfort.
- TESE: 3–5 days, with mild swelling or soreness.
- MicroTESE: 3–7 days, with careful aftercare to ensure optimal healing.
- Cost Considerations:
- TESA: Most affordable due to its simplicity.
- TESE: Moderately priced, balancing invasiveness and effectiveness.
- MicroTESE: Higher cost due to specialized equipment and expertise, but justified by superior outcomes in complex cases.
- Best Use Cases:
- TESA: Ideal for obstructive azoospermia with confirmed sperm production.
- TESE: Suitable for both obstructive and non-obstructive cases but less precise than microTESE.
- MicroTESE: Gold standard for non-obstructive azoospermia, especially when previous retrieval attempts have failed.
Cyprus IVF Centre evaluates each patient’s condition to recommend the most effective method, ensuring compliance with ethical standards and avoiding unnecessary procedures. For UK and Northern Ireland patients, the clinic provides clear information to align with HFEA guidelines, which emphasize informed consent and medical necessity.
Which Sperm Retrieval Procedure Should You Choose?
Choosing the right sperm retrieval procedure depends on several factors, including the cause of infertility, medical history, and fertility goals. Here’s a guide to help you decide, with insights from Cyprus IVF Centre:
- Consider Your Diagnosis:
- If you have obstructive azoospermia (e.g., post-vasectomy or congenital blockages), TESA may suffice due to its simplicity and high success rate.
- For non-obstructive azoospermia (e.g., genetic conditions or testicular failure), microsurgical testicular sperm extraction is recommended, as it offers the best chance of finding viable sperm.
- TESE may be a middle ground for cases where TESA fails but microTESE isn’t immediately necessary.
- Evaluate Sperm Production: Hormone tests (e.g., FSH, testosterone) and imaging (e.g., ultrasound) can indicate whether sperm production is occurring. MicroTESE excels when production is patchy or minimal, while TESA works best with normal production.
- Previous Treatment Outcomes: If prior attempts with TESA or TESE were unsuccessful, microTESE is often the next step due to its precision. Cyprus IVF Centre reviews past results to avoid repeating ineffective procedures.
- Partner’s Fertility Plan: Sperm retrieval is typically paired with IVF/ICSI, so the female partner’s treatment timeline (e.g., egg retrieval) influences the choice. MicroTESE allows for fresh or frozen sperm use, offering flexibility.
- Budget and Accessibility: While TESA is more budget-friendly, microTESE’s higher success rate may reduce the need for repeat procedures, saving costs long-term. Cyprus IVF Centre offers transparent pricing and financing options to ease financial burdens.
- Ethical and Regulatory Factors: In the UK and Northern Ireland, the Human Fertilisation and Embryology Authority (HFEA) regulates assisted reproduction, requiring procedures like microTESE to be medically justified. Cyprus IVF Centre ensures all treatments meet international ethical standards, providing documentation for patients returning home.
Ultimately, the decision should be made in consultation with a fertility specialist. Cyprus IVF Centre offers virtual and in-person consultations to assess your needs, ensuring the chosen procedure aligns with your medical profile.
Microsurgical testicular sperm extraction at Cyprus IVF Centre offers a beacon of hope for men facing infertility, providing a precise and effective way to retrieve sperm for IVF or ICSI. By understanding when microTESE, TESA, or TESE is appropriate, couples can make informed decisions tailored to their unique circumstances. With its commitment to affordability, expertise, and patient-centered care, Cyprus IVF Centre stands as a trusted partner in the journey to parenthood, adhering to ethical and regulatory standards worldwide.
